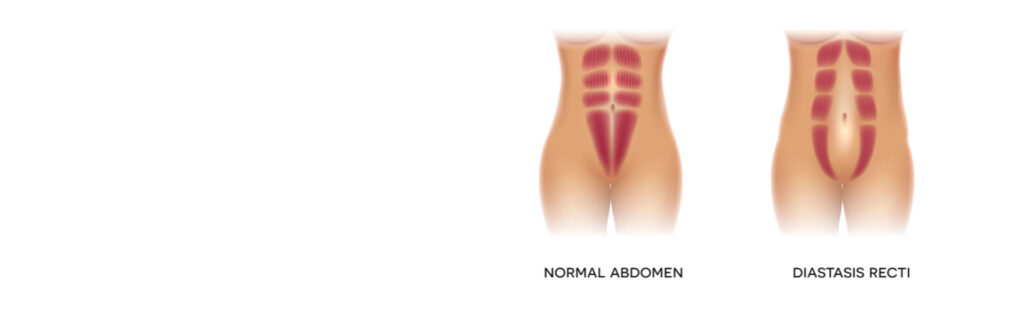
While this is one of the most common questions I hear from mothers, let me begin by stepping back and describing what, exactly, a rectus diastasis is. Beneath your abdominal skin is some superficial, or “subcutaneous” abdominal fat. Below this lies your abdominal wall. The abdominal wall consists of a series of muscles bound together by tough connective tissue called “fascia.” The abdominal organs, surrounded by deep, or “visceral” fat can be found under the abdominal wall. The muscles in the midline, the core of the abdominal wall, are called the “rectus abdominis” muscles. These are long, thick muscles that run in a pair up and down the length of your abdomen and, when developed, give the appearance of a “six pack.”
During pregnancy, as the uterus grows to accommodate a developing baby, multiple anatomic changes occur to accommodate this expanding structure. Most relevant to this conversation, the rectus muscles, which run up and down the midline of the abdominal wall, can be pushed apart and separated from one another to allow the abdominal wall to stretch. A thin, weak vestige of connective tissue is left behind where the rectus muscles were pushed apart. Deep abdominal fat can push this week connective tissue outwards creating a bulge that is present even after pregnancy. This bulge is called a rectus diastasis or diastasis recti.
The good news about a rectus diastasis is that you do not need to do anything about it at all unless it is bothering you. Symptoms from a rectus diastasis can include core weakness, back pain, and pelvic floor dysfunction leading to incontinence. It can also cause the appearance of a lower abdominal wall bulge. If you do decide you want to correct your rectus diastasis, you may be able to achieve some symptomatic relief with targeted core exercises and specialized physical therapy – there is not clear data on the efficacy of these approaches, but some folks are reporting positive experiences. However, a severe diastasis can prohibit you from participating from a core regimen in a meaningful way.
Abdominoplasty (more on that here) offers a definitive treatment for rectus diastasis. In this procedure, the rectus abdominis muscles are identified. The central separation between these muscles is then outlined. Sutures are used to repair the diastasis and reattach the rectus abdominis muscles in the midline. This approach repairs the biomechanical basis for the symptoms of rectus diastasis and also repairs the lower abdominal bulge.
What causes a rectus diastasis?
In our practice, the most frequent cause of rectus diastasis, and we see this all the time, is pregnancy because during pregnancy the uterus grows and expands to accommodate the developing fetus. And as this happens, it often needs to make more room for itself than the rectus muscles are providing. So the growing uterus can essentially stretch out the abdominal wall and separate the rectus abdominis muscles from one another and this results in a rectus diastasis.
Is a rectus diastasis the same thing as a hernia?
No, a rectus diastasis is not a hernia. The difference here is that a rectus diastasis is a separation of the rectus muscles, which leaves behind a weakened area of connective tissue between these muscles and the abdominal wall itself does remain intact, although it is weakened. In a hernia, and there are several kinds of hernia, but for the sake of this discussion were focusing on an abdominal hernia, there is actually a break or a hole in the abdominal wall, which can allow the deeper abdominal contents and visceral fat to bulge into or herniate into more superficial anatomical layers.
Can a rectus diastasis get worse over time? Yes. If you continue to place strain on your abdominal wall, either with further pregnancies or heavy lifting or anything else that can work to separate the rectus abdominis muscles from one another, the rectus diastasis can continue to evolve and worsen over time.
Is a rectus diastasis permanent? Unless steps are taken to address or fix a rectus diastasis it will remain permanently. These do not resolve or get better on their own.
Can a rectus diastasis be fixed?
Yes, it can. And we’ll get into that in a little bit more detail in a moment.
Do you need to have surgery to fix a rectus diastasis?
That’s a bit more of a complicated question. And the reason is that there are some physical therapy maneuvers that can improve a rectus diastasis and help with core strength. And while in mild cases this therapy may significantly improve your core strength it will not actually fix the anatomical basis of the rectus diastasis.
Similarly, another non-surgical way to fix a rectus diastasis is with EMSCULPT. And this is a procedure we’ve discussed at length in other episodes, but essentially it uses highly focused electromagnetic energy or HIFEM to stimulate the abdominal muscles. In fact, it can generate up to 20,000 contractions in about 30 minutes. EMSCULPT can grow your rectus abdominal muscles, increase their muscle mass and in doing so it can actually reduce the width of a rectus diastasis by several percentage points.
However, again, I would not rely on EMSCULPT to treat a severe rectus diastasis, but in a mild case, it could offer some improvement. So unfortunately the only way to definitively manage a rectus diastasis is with surgery. And we do this in a tummy tuck or abdominoplasty, which we’ve also discussed in an earlier episode. But as far as it pertains to rectus diastasis during a tummy tuck or abdominoplasty, we actually identify the borders of the rectus abdominis muscles in the midline and then we actually sew those medial borders of the rectus diastasis muscles together in a process called plication.
Conclusion
So while a rectus diastasis is a very common problem and it can cause functional issues by making you feel like you have a weak core, or aesthetic issues by causing an abdominal bulge and making it very difficult to achieve a flat abdomen, rectus diastasis is fairly easily managed in minor cases by other physical therapy or with EMSCULPT and in a more severe cases with an abdominoplasty.



